Haemoglobinopathies are a group of hereditary diseases that result as a consequence of defect(s) in the genes responsible for the synthesis of haemoglobin. Depending on the molecular defect, haemoglobinopathies may be classified as either thalassaemias or structural hemoglobin variants.
Haemoglobin (Hb) is a protein found in the erythrocytes (red blood cells) with the primary function to transport oxygen from the lungs to the rest of the body and return carbon dioxide from tissues to the lungs.
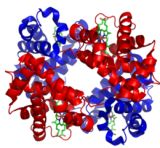
The structure of Haemoglobin comprises of four polypeptide chains known as globins, each containing a heme group and 141 or 146 amino acids forming seven or eight helical regions separated by non-helical segments.
Normal haemoglobin types include:
- Hb A – the predominant form in adults (95%-98% of Hb) consists of two alpha (α) protein chains and two beta (β) protein chains (α2β2)
- Hb A2 – typically 2%-3% of Hb in adults; has two alpha (α) and two delta (δ) protein chains (α2δ2)
- Hb F – the primary haemoglobin produced by the fetus during pregnancy, usually falling to a low level shortly after birth and making up to 2% of Hb found in adults; has two alpha (α) and two gamma (γ) protein chains; (α2γ2)
Alterations in the amino acid composition of globin chains, or the rate of their production, can occur through genetic mutation. These changes may, in some cases, produce clinically significant effects and are known as haemoglobinopathies & thalassaemias.
Both haemoglobinopathies & thalassaemias are disorders of haemoglobin, with haemoglobinopathies resulting in abnormal structure of the globin molecules and thalassaemias typically resulting in underproduction of normal globin proteins, often through mutations in regulatory genes. The two conditions may be present simultaneously.
Haemoglobinopathies
The abnormal haemoglobin types which result from haemoglobinopathies are known as Haemoglobin Variants (HbV), the most prevalent of which include:
- Hb S
- Hb C
- Hb E
- Hb D-Punjab
- Hb O-Arab
- Hb G-Philadelphia
Although many HbV do not cause any detectable pathology, particularly when heterozygous, those that do affect red-cell function typically result in anaemia. The most prevalent of these is Sickle Cell Disease, which occurs when there is homozygosity for the mutation that causes HbS. In heterozygous people, who have only one sickle gene and one normal adult haemoglobin gene, it is referred to as HbAS or ‘sickle cell trait’. SCD is characterised by erythrocytes that assume an abnormal, rigid, sickle shape which decreases cell flexibility and leads to various complications.
Thus pre-natal screening for HbS – and other HbV – is a commonly used tool to identify parents at risk of having a child with a homozygous condition.
Thalassaemias
In thalassemia the genetic defect, which could be either mutation or deletion, results in reduced rate of synthesis – or no synthesis – of one of the globin chains that make up hemoglobin. This can cause the formation of abnormal hemoglobin molecules, thus typically causing anemia.
Thalassemias are historically revalent in populations that evolved in humid climates where malaria was endemic and as such may confer a degree of protection against malaria. They are particularly associated with people of Mediterranean & Arabic origin. There are two major forms of the disease, alpha- and beta- as described below.
Alpha-thalassemia
The α thalassemias involve the genes for HbA1 and HbA2, leading to decreased alpha-globin production and a subsequent excess of β chains in adults and γ chains in newborns. The excess β chains form unstable tetramers (known as HbH), which have abnormal oxygen dissociation curves.
Beta-thalassemia
Beta thalassemias are due to mutations in the HBB gene on chromosome 11, with severity depending on the nature of the mutation.
- If they prevent any formation of β chains, the most severe form, they are known as β thalassemia major (βo).
- If some β chain formation occurs, they are they are known as β thalassemia intermediate (β+).
In both cases there is a relative excess of α chains although, unlike α-thalassaemia, they do not form tetramers but instead bind to the red blood cell membranes producing membrane damage and potentially toxic aggregates.
Prevalence, Screening & Detection
Although haemoglobinpathies & thalassaemias are primarily found in Mediterranean, Arabic & Asian countries, due to worldwide emigration they are becoming increasingly prevalent globally.
As such there is a need for both the accurate quantification of HbF and HbA2 to allow for the screening of ß-thalassemia in addition to reliable separation and identification of common and clinically significant structural hemoglobin variants.